Reverse total shoulder replacement is an advanced surgical technique tailored specifically for rotator cuff tear arthropathy, a condition characterized by both shoulder arthritis and a torn rotator cuff.
The shoulder joint comprises the union of the upper arm bone’s head (humerus) and the shoulder socket (glenoid). The rotator cuff, a group of four tendons, connects the humerus head to deeper shoulder muscles, providing stability and mobility to the joint.
When the rotator cuff tears, it can lead to shoulder joint wear and tear, resulting in arthritis. Traditional surgical approaches, such as total shoulder joint replacement, have proven largely ineffective in addressing rotator cuff arthropathy.
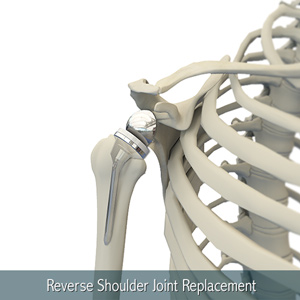
Conventional shoulder replacement entails replacing the humerus’s ball with a metal component and the glenoid cavity of the shoulder blade with a plastic socket. However, if used to treat rotator cuff arthropathy, this method may fail due to implant loosening caused by the torn rotator cuff. Hence, the development of reverse total shoulder replacement specifically addresses such cases.
In reverse total shoulder replacement, the artificial components’ placement is inverted. Essentially, the humeral ball is positioned within the shoulder blade’s glenoid cavity, while the plastic socket is affixed atop the arm bone. This design leverages the deltoid muscle’s strength to compensate for the torn rotator cuff.
Symptoms
Symptoms of rotator cuff arthropathy often include nocturnal shoulder pain and weakness, particularly in overhead activities.
Symptoms
Candidates for reverse total shoulder replacement typically exhibit a completely torn rotator cuff that is challenging to repair, evidence of cuff tear arthropathy, prior unsuccessful shoulder replacements, severe shoulder pain, and limited overhead functionality despite various treatments.
Procedure
During the surgery, conducted under general anesthesia, the surgeon makes an incision over the affected shoulder to access the joint. The humerus is separated from the scapula’s glenoid socket, and the arthritic portions of both bones are removed to prepare for artificial component insertion. These components include a metal ball screwed into the shoulder socket and a plastic cup cemented into the upper arm bone, securing the artificial components in place. The joint capsule is stitched, tissues are approximated, and the wound is closed with sutures.
Post-operative care
Post-operative care involves early mobilization, typically allowing patients to get out of bed on the same day as the surgery, with hospital stays lasting 1-2 days. General instructions include medication adherence, gentle range of motion exercises, recommended physical therapy for shoulder strengthening and flexibility improvement, avoidance of overhead activities for at least 6 weeks, refraining from using shoulder muscles to push oneself up, and avoiding heavy lifting.
Risks and complications
Potential risks and complications associated with reverse total shoulder replacement surgery include infection, joint dislocation or instability, humerus or scapula fractures, nerve or blood vessel damage, deep vein thrombosis, wound irritation, arm length discrepancies, and component wear.