The shoulder represents a remarkably flexible joint facilitating a wide array of arm movements. It operates as a ball and socket joint, where the upper arm bone (humerus) connects with the shoulder blade’s (scapula) socket, known as the glenoid. To prevent friction between these articulating bones, cartilage covers their surfaces while being lubricated by synovial fluid. Surrounding tendons and ligaments offer stability and strength to the shoulder joint.
When cartilage suffers damage, bones begin to rub against each other, resulting in discomfort, swelling, and restricted movement, a condition commonly known as osteoarthritis.
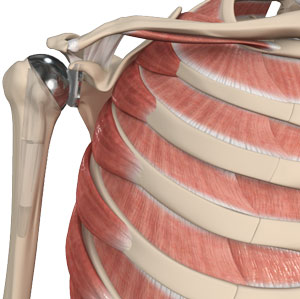
Total shoulder replacement surgery is a corrective measure to alleviate these symptoms. This surgical procedure entails removing the damaged components of the shoulder joint and substituting them with artificial prostheses. Complete replacement of both the humeral head and the socket constitutes a total shoulder replacement.
Indications
Indications for this surgery typically arise in cases of osteoarthritis or rheumatoid arthritis where conventional treatments like medication, therapy, injections, and lifestyle adjustments fail to provide relief. Surgery becomes a recommendation when patients experience:
- Severe shoulder pain hindering daily activities
- Moderate to severe pain even during rest
- Weakness and/or restricted motion
Diagnosis
Diagnosis involves a comprehensive evaluation of the patient’s medical history along with a physical examination of the shoulder joint’s mobility and pain levels. Imaging techniques such as X-rays or MRI scans are often employed to assess the extent of damage.
Procedure
The surgical procedure is conducted under regional or general anesthesia. An incision is made over the affected shoulder, exposing the joint by separating underlying muscles. Surgery may be performed via open surgery, involving a sizable incision, or minimally invasive techniques utilizing small incisions for arthroscope insertion—a tool comprising a thin tube with a camera and light source, alongside surgical instruments.
The damaged humeral head is excised, and the humerus bone is hollowed out and filled with cement. A metal ball with a stem is then inserted into the humerus. Subsequently, the arthritic portion of the socket is prepared, and a plastic glenoid component is secured within the shoulder bone. Post-implantation, the joint capsule is sutured, and the incision is closed.
Post-operative care
Post-operative care involves prescription pain management and antibiotics to mitigate pain and prevent infections. Patients may require slings or casts to secure their arm post-surgery. Physical therapy, initiated soon after the procedure, plays a crucial role in enhancing shoulder strength and mobility. Patients can gradually resume gentle daily activities within two to six weeks post-surgery.
Risk and complications
Potential risks and complications associated with this major surgery involved:
- Severe shoulder pain hindering daily activities
- Wound infections
- Dislocation necessitating further surgery
- Vascular
- Neural or muscular damage
- Inadequate pain relief
- Pulmonary embolism
- Prosthesis wear and tear.